Optimising Heart Health
DISCOVER MORE ABOUT WORKING WITH A DIETITIAN
SUPPORTING YOU IN FINDING OPTIMAL HEART HEALTH
We are all very aware of the importance of our heart and entire cardiovascular system, but as a nation we are not doing a very successful job of having good heart health. Strokes and heart disease are responsible for about 25% of all deaths in the western world. Both conditions are referred to as ‘silent killers’ because the first symptoms or signs in many cases is a fatal event.
Heart health and cardiovascular disease is influenced by a multitude of factors, genetrics to more modifiable factors such as the foods you eat, your lifestyle as well as stress management.
If you’re concerned about your cardiovascular health, our team of heart health specialists are here to support you in creating a personalised nutrition and lifestyle plan, to keep you and your heart healthy.

POSSIBLE SIGNS AND SYMPTOMS
The first indication that there may be a problem could be flagged in a routine screening of cholesterol or blood pressure makers with a GP.
However, if you aren’t having regular screenings or experience many of the dietary and lifestyle risk factors, heart disease can often go undetected, until a heart health crisis.
Symptoms can include
- Chest pain, chest tightness, chest pressure and chest discomfort (angina)
- Shortness of breath
- Pain, numbness, weakness or coldness in your legs or arms if the blood vessels in those parts of your body are narrowed
- Pain in the neck, jaw, throat, upper abdomen or back
Major risk factors include
- Smoking
- High blood pressure
- Diabetes
- Physical inactivity
- Prolonged stress
- Insulin resistance
- Chronic inflammation
HEART HEALTH SPECIALISTS
It is hard to believe that the idea of heart disease being reversible through modifiable lifestyle choices was a radical one just 30 years ago. Today, many medical bodies emphasise the value of lifestyle interventions, and yet the encouragement of this from doctors’ offices is likely not as thorough as it could be.
When we consider the risk factors we start to understand the importance of diet and lifestyle in the management of cardiovascular health. Healthy lifestyle management signals is a powerful and necessary therapy for individuals at all points along the continuum between vibrant health, dysfunction, pre-disease and diagnosed disease. Ensuring safe and sustainable weight loss and weight management may be an important factor in keeping a healthy heart.
How our Heart Health Specialists can support you
Dietary patterns have changed dramatically in Western countries over the last 100 years. With few exceptions, studies have shown that these changes have been harmful for the populations that consume them, leading to a higher risk of nearly all chronic disease.
Our team of heart specialist nutritional therapists and dietitians will work with you to adapt your diet in a personalised way. Some of the areas they may work with include
- Saturated Fats – A review of the data has shown that diets consisting of saturated fat, trans-fatty acids, high glycemic load and low folate levels are linked to increased heart disease; while diets consisting of polyunsaturated fats, omega-3 fatty acids, low glycemic load and high in fruits and vegetables consistently lower cardiovascular risk in populations that consume them.
- Fasting Intermittent fasting has also been shown to improve cardiovascular health by decreasing oxidative stress and inflammation, improving mitochondrial function, cholesterol, triglycerides, insulin sensitivity and blood pressure.
- Micronutrients Nutrients that are essential for optimal heart health include omega fatty acids, magnesium, CoQ10, Alpha-lipoic acid, Vitamin B3, Vitamins, D, E and K and more.
We offer support from a functional perspective, and understand that statins are not the only answer to managing your heart health.
FUNCTIONAL TESTING OPTIONS
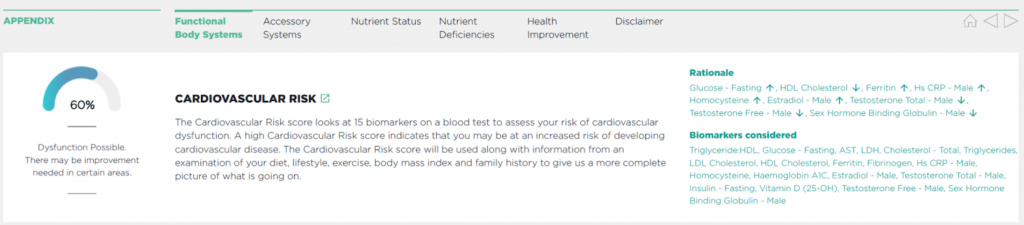
The risk of developing heart disease has traditionally been assessed by measurement of LDL-C (low-density lipoprotein cholesterol; the carrier of “bad” cholesterol) and HDL-C (high-density lipoprotein cholesterol; the carrier of “good” cholesterol).
Recent studies demonstrate that about 50% of heart attacks and strokes occur in people with ‘normal’ cholesterol levels. This suggests that many people at risk are presumed low-risk because they have “normal” or controlled cholesterol levels. Therefore, routine cholesterol tests may fail to fully identify people at risk of heart attack and stroke.
Although it is essential to assess your cholesterol levels, adverse cardiac events (such as heart attack, stroke or death) have been associated with inflammation, specifically vulnerable plaque related to increased white blood cell activation.
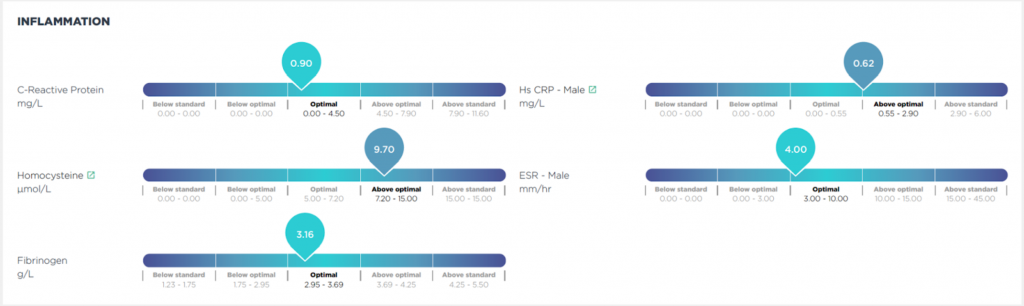
More comprehensive cardiovascular profiles including markers of inflammation such as homocysteine, myeloperoxidase, oxidised LDL and F2-Isoprostanes better help evaluate cardiovascular risk. These indicators help us understand more specifically the development of metabolic or cardiovascular disease, and the formation of vulnerable plaque which may contribute to an increased risk of an adverse event.
Below we have included an example of some of the markers we can test for, produced in an easy to understand report.


FAQs
Everyone is different, and the number of consultations can depend on the length of time you have had symptoms, how motivated you are for change, and how regularly you want your sessions. On average we recommend an initial consultation and 2 to 3 follow-up sessions over a 3 month period. Many of our clients choose one of our Online Health Packages.
Yes, certainly. Your heart health specialist will take a detailed health history and assessment of your current medications and supplements during the initial consultation, and will take this into consideration when suggesting any dietary and lifestyle recommendations. We can also offer private, functional testing to assess your cardiovascular health, interpret the results and talk the results through with you.
Our prices vary depending on which practitioner you see and the length of the consultation. We like to be transparent about our fees, and you can take a look here.
Our Heart Health clinic is based at the King Edward VII Hospital, however most of our practitioners work remotely online. This means we can support you wherever you are in the world.
NEXT STEPS
If you resonate with any of these symptoms and would like some support, please book a complimentary call with our friendly assessment team.
They will talk through your health goals and symptoms, and recommend one of our nutrition team that specialises in balancing hormones.
